Popular herbal medicines for COVID-19 have been reported to adversely affect the liver and kidney – at times, even leading to death.
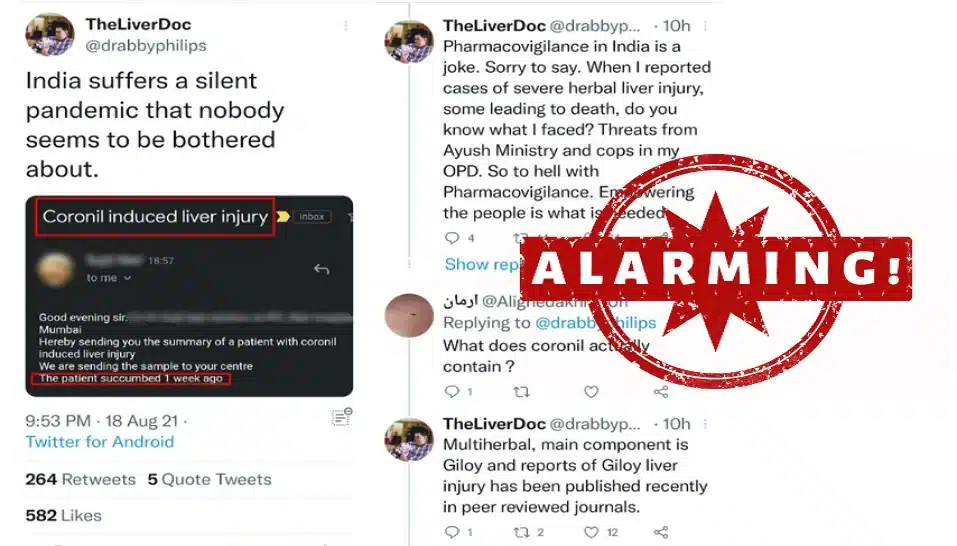
Recently, a tweet by Dr. Cyriac Abby Philips, Hepatologist from The Liver Institute, Center of Excellence in GI Sciences, Rajagiri Hospital in Kerala, garnered a lot of traction as he put the spotlight on the “silent pandemic that nobody seems to be bothered about”. His concern was about the growing cases of liver injuries induced by popular herbal remedies, particularly to treat COVID-19. Patients have been succumbing to liver failure after an overdose of herbal medicines and concoctions.
A number of herbal preparations, touted as “immunity-boosting” or “tested and verified medicines”, are easily available over the counter. While none of them have yet been scientifically proven to be beneficial against COVID-19, multi-ingredient herbal preparations have been reported to adversely affect liver and kidney – at times, even leading to death.
“Commonly used herbal preparations contain curcumin (from turmeric), ashwagandha, aloe vera, Tinospora cordifolia or Giloy and green tea extracts. Green tea extract infusions have been associated with severe liver injury,” said Dr. Philips when contacted by First Check.
In some cases, surgeons have reported incidents where patients previously taking herbal medicines bled profusely during surgery. “Some herbs contain substances known as coumarinoids, which are naturally occurring blood thinners. Excessive consumption of coumarinoid-rich herbs or ingestion of such herbs by persons who are already on blood thinners lead to bleeding complications. This is well documented with fenugreek or methi, the seeds of which are used as decoctions by persons with diabetes without proper evidence,” explained Dr. Philips.
The liver is an organ that detoxifies any harmful substance and converts it into waste that is eliminated from the body. A recent paper in a peer-reviewed journal has reported a case study on six patients affected with liver damage after taking a heavy dose of herbal medicines. Most herbal medicines are not approved by any regulatory bodies. This means, those medicines are not tested rigorously in laboratories and in clinical trials.
For a majority of herbal medicines, the formulations and dosing are decided by pharmaceutical companies themselves. Such companies also use marketing gimmicks and label the packaging with buzzwords such as “immunity booster”, “100 % natural”, and the like.
Herbal concerns
One major problem lies in the gap in understanding what exactly herbal medicines do. Herbal medicines may provide symptomatic relief against respiratory ailments, but they do not ‘cure’ diseases like COVID-19. Secondly, if something is ‘natural’, it doesn’t necessarily mean it is safe.
In the case of COVID-19, the only medicine which the FDA has approved so far is Remdesivir. The approval means that Remdesivir has been rigorously tested in laboratory tests, on animals, and on tens of thousands of humans to check if the drug is safe and is superior to an existing treatment or a placebo. Do we have such validated studies for testing the safety or efficacy of any herbal medicines that claim to cure or prevent COVID-19?
Additionally, people also use herbal medicines along with modern medicine, in an effort to “improve the clinical effect”. “This integration (of modern and herbal medicine) is quite concerning and fraudulent. The herbal medicine might turn out to be a placebo and along with the proper modern medicine benefiting, people will falsely attribute effectiveness to the herbal medicine. Certain herbal medicines when used along with modern medicines can either worsen toxicity of modern medicine, reduce effectiveness of modern medicine, or cause herbal related side effects,” cautioned Dr. Philips.
In India, the use of herbal medicines is deeply rooted in faith and religious or traditional beliefs, rather than scientific evidence. It is important to seek the evidence for any claim, rather than blindly following the belief system it is based on. Shockingly, doctors, scientists as well as fact-checkers trying to debunk unscientific claims on herbal medicines have been trolled online, harassed as well as received death threats!
“Once the mind can be trained to focus on the evidence for a particular form of treatment,” noted Dr. Philips, “and not the belief or the faith system that guides that treatment, it becomes easier for one to openly discuss the merits and demerits of using herbal supplements”.
(The author is a science educator as well as member of First Check and the Indian Scientists’ Response to COVID-19 team, with the Hoaxbusters’ group.)

















Add Comment