Based on the data released by China, ventilators played a crucial role in saving lives of critically-ill COVID-19 patients. Now, as the number of cases surge in India, is the country of 1.3 billion people ready to cope with the increasing demand for lifesaving machines, finds Dayawanti Punj.
In a bid to contain the spread of deadly novel coronavirus, most countries across the globe have locked down their borders and imposed travel bans. But, the central Chinese city of Wuhan, where the deadly virus had originated late last year is easing down on restrictions and containment measures as the community infection rate in the country has gradually gone down.
Although the epidemic of COVID-19 in China is not yet over, it has been reported that more than half of all new cases in the country since the start of April have come from abroad.
In addition, to be at the forefront to develop a vaccine against coronavirus, China has not only tightened its grip on coronavirus research, but the country is also releasing various studies on COVID-19 besides sharing their experience in epidemic response and medical treatment with the international community.
Even medical professionals who have been treating corona patients worldwide are turning to findings from China to better understand the disease that has affected more than 200 countries and regions with over 1.13 million confirmed cases by April 5, 2020.
Multiple scholarly papers published on early transmission dynamics in Wuhan over the past few weeks highlight the need for mechanical ventilators during the peak of the epidemic.
It is reported that the need for a ventilator arises when patients show signs of severe oxygen deficiency in the body due to Acute Respiratory Distress Syndrome (ARDS) – known as hypoxemia. While it is a common complication of acute COVID-19, the most effective way to treat the condition is through the timely use of a mechanical ventilator. These ventilators are inserted into the throat, typically through an endotracheal tube, and artificially simulate the breathing process to increase oxygen levels in the body.
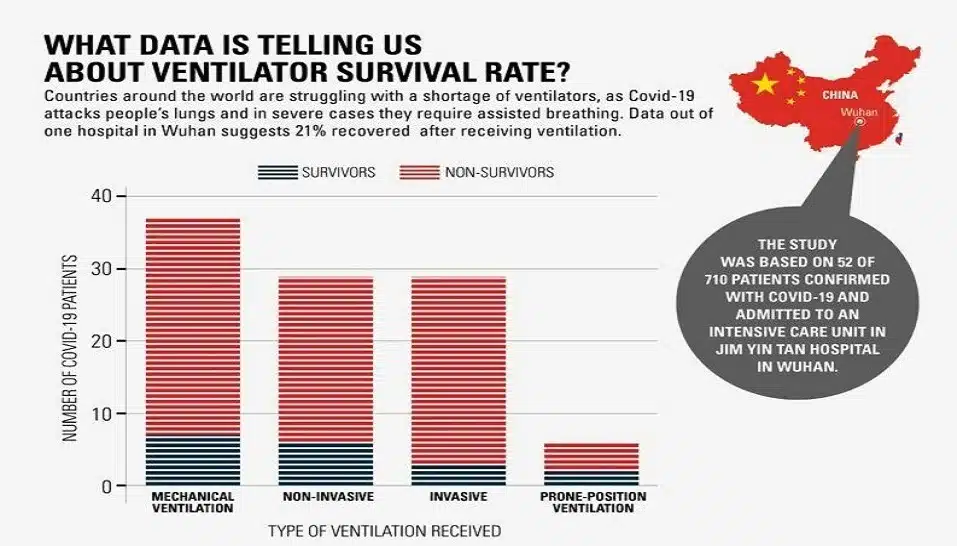
Furthermore, an observation based on critically-ill COVID-19 patients in Wuhan, published in Lancet reports that the average survival rate of 21.6 percent critical care patients was dependent on ventilation treatment. Also, the paper highlights that the severity of SARS-CoV-2 pneumonia poses great strain to the hospital’s critical care resources, especially if they are not adequately resourced. This proves that ventilators are an invaluable medical resource in the fight against coronavirus.
Besides, if we go by another report published in Anesthesiology, an official journal of the Association of Anaesthetists, it is estimated that approximately 3.2 percent of 80,409 diagnosed cases in mainland China required intubation and invasive ventilation at some point in the disease course. The report is based on China’s data as released on March 4, 2020.
According to these statistics, about 2,600 patients needed invasive ventilators at the beginning of January, and according to the WHO report, the virus in Wuhan had not reached its peak until late January.
Though we do not have recent data detailing the total number of patients who received intubation and invasive ventilation during COVID-19 treatment, nonetheless, we can attempt to interpret the severity of the situation based on the available data.
India’s race against ventilators
As coronavirus has spread across continents, countries across the globe are experiencing this rising need for ventilators, and the race to acquire as many units as possible in a market already saturated with demand has commenced.
China’s dependence on a ventilator to treat a large number of its COVID-19 patients is a cautionary tale for India. The country with a population of 1.3 billion, by most estimates, only has 40,000 functional ventilators. This will meet just a fraction of the potential demand.
While highlighting the urgency to procure ventilators, Lav Aggarwal, Joint Secretary, Ministry of Health during a press briefing said, “In 2019, government-run hospitals were the biggest procurers of ventilators, with the public sector HLL Lifecare Ltd placing an order for 1,286 units, and Maharashtra, Hyderabad, and Telangana placing separate orders, including for cheaper ambulatory ventilators. After the COVID-19 outbreak, they have ordered for the acquisition of 1,200 units.”
Though the government is doing its bit, however, if industry experts are to be believed India will need to increase the number of ventilators exponentially as the virus spreads.
In fact, to cope up with the growing demand, the government has also allowed the import of second-hand or used ventilators. In a memorandum dated April 1, the ministry of environment, forest and climate change relaxed the import policy to facilitate the use of second-hand ventilators by hospitals, which otherwise falls under the category of goods prohibited for import under Schedule VI of Hazardous and Other Wastes (Management and Transboundary Movement) Rules, 2016.
Also, the government has urged many manufacturers to reconfigure their factories to produce this life-saving, and now essential, commodity instead of their own products, but the barriers to production are costly, much like the ventilators themselves. On average, a ventilator costs Rs 3-4 lakh per unit. Therefore, monetary obstacles and production delays could lead to a potentially catastrophic healthcare crisis, as it did in other hard-hit countries.
What did the Government of China do to mitigate the ventilator shortage in Wuhan?
Going by Wuhan’s experience, the Chinese Government took multiple steps to meet the demand for ventilators. This was achieved largely through lowering tariffs on imports and urging manufacturers to boost in-house production.
In mid-February, the Ministry of Commerce of China announced a tariff cut on $75 billion (Rs 5,000 crore) worth American-made goods that included medical supplies.
In January and February 2020, the US exported approximately $27 million worth of ventilators to China, according to the most recent foreign trade data available from the US Census Bureau. The majority of the country’s ventilator needs were met by its domestic manufacturers though.
According to a statement released by China’s Ministry of Industry and Information Technology in February 2020, a shipment of approximately 14,000 non-invasive ventilators, and 2,900 invasive mechanical ventilators were carried out by 21 Chinese manufacturers to the Hubei region, where the city of Wuhan is located. Apart from this, two new temporary hospitals (with 2600 beds that were dedicated completely to COVID-19) were constructed, and there was a surge in the number of hospital beds available across the city.
Despite the government’s actions, their reaction to the ventilator crisis was delayed. According to the report of the WHO-China joint mission, the epidemic curve had reached its peak in February, after which it began to plateau. The majority of the ventilator shipments, on the other hand, were delivered to Hubei in late February to beginning March, when situation started to get better.
Ultimately, China ended up with 80,000 COVID-19 active cases, out of which 9,000 were critical care patients.
So, what can we learn from Wuhan’s experience? Clinical studies were conducted across hospitals in Wuhan where COVID-19 patients were treated over the course of January-February 2020 when the outbreak was at its peak in the region.
Considering the universality and extent to which COVID-19 has spread, these samples- which were crafted to be representative of the critical care patient population of Wuhan- could also be indicative of the trajectory followed by hospitals in other regions severely affected by the virus across the globe.
The ventilation data from one such study from January 2020, at Jin Yin Tan Hospital is given. This clinical study also provides survival data on each of these treatments for the 52 critical care patients observed.

The study conducted on 52 critically-ill adult patients who were residents of Wuhan gives an indication as to the effectiveness of different ventilation treatments. For example, 31 (71%) patients in the study received mechanical ventilation, 29 (56%) received non-invasive ventilation (respiratory support through a nasal or face mask), 22 (42%) received invasive ventilation (where an endotracheal tube is inserted to artificially stimulate breathing), and 6 (11.6%) received prone-position ventilation, where the patient receives ventilation invasively while lying on their stomach. And, because many of these patients received multiple treatments, hence these proportions don’t add up to 100 percent.
While more patient-specific analysis into the clinical data from Wuhan by medical professionals is certainly required, these studies provide key insights into the effectiveness of multiple treatments on critical-care coronavirus patients.
Now that Wuhan and most of the mainland is recovering from the epidemic, China has resumed its role as one of the biggest exporters of ventilators. Manufacturers are currently working to fulfill the exponentially increasing foreign demand from countries including the US, Italy, and Spain, which is roughly estimated to be about 20,000 units ordered, over the course of the next few months.
Disclaimer: This story is based on data released by the Health Ministry of India until April 5, 2020.