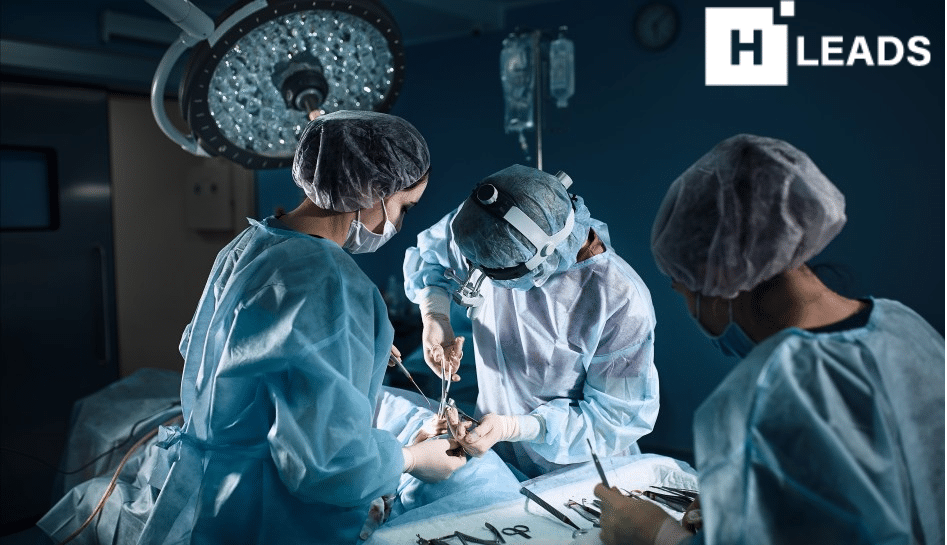
The Deep Brain Stimulation (DBS) involves implanting electrodes in the patient’s brain to regulate her mood
A 38-year-old woman from Australia, who had been struggling with depression for the past 26 years, recently underwent a groundbreaking psychiatric operation in Mumbai, making her the first patient to receive this treatment in India since the passage of the new Mental Healthcare Act in 2017.
The Deep Brain Stimulation (DBS) surgery involves implanting electrodes in the patient’s brain to regulate her mood. The DBS is a minimally invasive procedure that has been shown to be effective in treating a variety of neurological conditions, including Parkinson’s disease, essential tremor, and Obsessive-Compulsive Disorder (OCD). It is also being increasingly used to treat severe depression that has not responded to other treatments.
Under the provisions of the new Act, psychosurgery can only be performed with informed consent from the patient and approval from a specially appointed state mental health board. Previously, such requests were evaluated by a hospital board.
However, prior to the enactment of this law, a similar surgery took place in Mumbai in October 2013, when a 26-year-old Australian became the first patient to undergo brain surgery to manage severe depression. He had been suffering from severe depression for six years, experiencing suicidal thoughts. He approached Mumbai’s Jaslok Hospital, where the medical team, including psychiatrists, neurosurgeons, and a neurologist, determined that he was an ideal candidate for the DBS, a procedure performed at only a few select centers worldwide.
The surgery in 2013 was carried out using local anesthesia and stereotactic guidance, with the patient fully awake throughout the procedure.
In the recent case, the patient had attempted various combinations of antidepressants and therapies without significant improvement. Despite being a trained occupational therapist, she had ceased working seven years ago due to her condition. Her brother said that she had tried 20 different antidepressants, often at higher doses than usual, and had also undergone electroconvulsive therapies (ECT) as well as cognitive and behavioral therapy, with limited benefit.
The procedure was conducted with the patient awake to allow for the mapping of responses while placing the electrodes. Doctors reported a significant reduction in the patient’s anxiety and a slight improvement in her mood during the surgery.
Mental Healthcare Act in 2017
The Mental Healthcare Act 2017 (MHCA) is a landmark legislation in India that aims to protect the rights of persons with mental illness and to provide them with access to quality healthcare services. Some of the salient features of the MHCA include:
- Decriminalizing suicide: The MHCA decriminalizes suicide attempt by a person with mental illness. This is a significant step towards reducing the stigma associated with mental illness and encouraging people to seek help.
- Providing for involuntary admission: The MHCA provides for involuntary admission of a person with mental illness in certain circumstances, such as when the person is a danger to themselves or others, or when they are unable to take care of themselves. However, the MHCA also safeguards the rights of the person by requiring that involuntary admission be authorized by a Mental Health Review Board (MHRB).
- Prohibiting certain treatments: The MHCA prohibits certain treatments for mental illness, such as unmodified electroconvulsive therapy (ECT), seclusion, and chaining. These treatments have been found to be harmful and ineffective, and their use is now restricted to only the most severe cases of mental illness.
- Enshrining the rights of persons with mental illness: The MHCA enumerates a number of rights for persons with mental illness, including the right to access mental healthcare services, the right to live with dignity, the right to confidentiality, and the right to legal aid. These rights are essential for ensuring that persons with mental illness are treated with respect and have the opportunity to live full and productive lives.
- Also Read: Men and women experience depression differently
















Add Comment