Given the decades of under-investment in the public health system and social health, India needs to swiftly marshal financial and human resources to tackle the pandemic. Apart from makeshift hospitals and isolation units, the country needs basic ventilators and PPE using indigenous design.
By Mahaveer Golechha
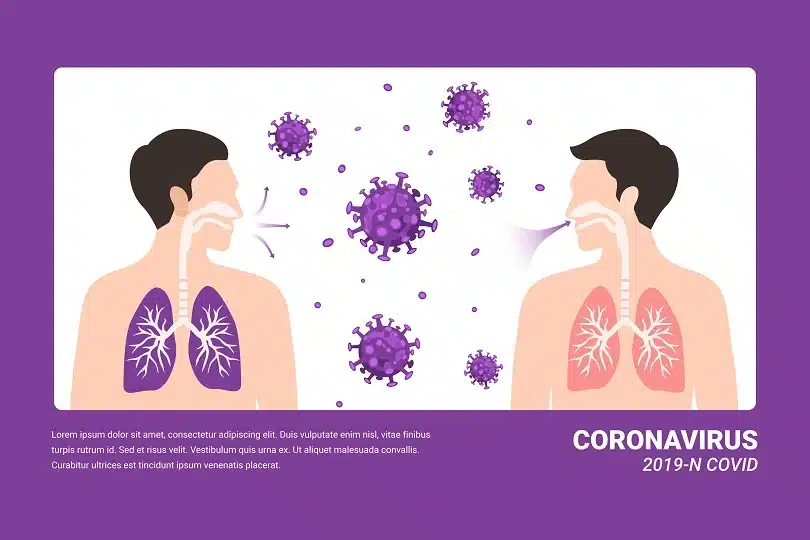
When the World Health Organization (WHO) declared COVID-19 a pandemic on 11th March 2020, it called for governments to take “urgent and aggressive action” to change the course of the outbreak. The future of the COVID-19 pandemic, the WHO stated, is dependent on the response of countries like India, which have a tremendous capacity to handle the coronavirus outbreak as it has a history of eradicating pandemics such as the small-pox and polio.
As the world’s second-most populous nation, India is experiencing an exponential increase in COVID-19 positive cases, with quite a few areas being declared as the red zone. In the coming weeks, the health infrastructure will be tested severely, with the number of new cases in the country increased by more than 1000 each day.
Window of opportunity
An analysis of medical infrastructure and other data of the top 10 affected countries shows that India lags far behind on the resources required to deal with a pandemic. Before the coronavirus outbreak hits its peak, it is necessary to use this window of opportunity to create an enormous, affordable, and accessible respiratory care infrastructure across the nation.
The rapid increase in the number of cases of COVID-19 in China, Italy, and Spain has highlighted how quickly respiratory care infrastructure can be challenged to provide adequate care. The significant number of patients who required a ventilator went on to die of respiratory failure, despite maximal support. Initial reports suggest that COVID-19 is associated with severe disease that requires intensive care in approximately five percent of proven infections.
India at this stage also needs a large number of makeshift hospitals and isolation units to treat COVID-19 patients as the existing healthcare facilities will not be sufficient if the number of COVID-19 cases surges in a pattern similar to Europe and the US.
Support indigenous designs
According to a Brookings report, if the number of cases spirals in India, it may need as many as 110,000-220,000 ventilators as early as mid-May. It estimated the number of ventilators today in the country at a maximum of 57,000. India is largely dependent on imported parts for ventilators and other critical care instruments. Most of the ventilator manufacturers in India have indicated their inability to ramp up production due to export restrictions on medical devices from China and Europe.
The government should support Indian R&D institutes or companies for producing basic ventilators using indigenous design and components. This would help local manufacturers to mass-produce ventilators so that we do not face a situation like Italy where people died for want of treatment. Therefore, the government should prepare for handling increasing numbers of patients with COVID-19, plans should be made at central and regional levels for how to manage optimally the potential surge in the need for respiratory care resources.
The personal protective equipment (PPE) is one crucial way to both stop the spread of COVID-19 and keep the frontline healthcare workers safe from the pandemic. There are concerns that if the lockdown is lifted and if the infection spreads, the lack of PPEs could be a major problem area for the government. Also, some reports highlighted the shortage of PPE across various states in India. If we will not be able to protect our health workers, there will be a double burden, a reduction in the number of human resources, and an increase in the number of cases on another side. The government should leverage the potential of Indian textile industries for ramping up production of PPE.
Need for ‘Board Eligible Specialists’
India has around 9.26 lakh doctors for a nation of 1.3 billion, of which less than 20,000 are trained in pulmonology, anaesthesiology, critical care, and emergency medicine – the key departments for respiratory care and active life-saving intervention.
Under the National Board of Examination (DNB), around 12,000 specialist doctors just finished their final year theory paper of specialty exams in anesthesia, medicine, pulmonology, cardiology, etc. and nearly 30,000 medical specialists are trained in vital specialties under Medical Council of India (MCI) annually. As in the USA, the Indian government can give the degree as ‘Board Eligible Specialist’, and later when they clear the final exam, they can be called ‘Board Certified Specialist’.
They would be an asset in this time of crisis. The government should also initiate standardised training in various domains, such as critical care, pulmonology, case management, infection control, safety testing, and isolation protocols. This will enhance comprehensive skills to respond effectively and make teams better prepared to deal with health emergencies in the ICU.
Address the gap
India has to move speedily, marshal its financial and human resources, and build temporary COVID-19 treatment facilities. The need of the hour is to procure necessary respiratory care equipment, including PPEs, hospital beds, oxygen-flow masks, and ventilators.
India will need to address the decades of under-investment in the public health system and social health, which may leave it struggling at this time of crisis. This could be an opportunity for India to strengthen its health infrastructure for the advancement of public health like never before.
(The author is Associate Professor and Acting Registrar at Indian Institute of Public Health Gandhinagar)