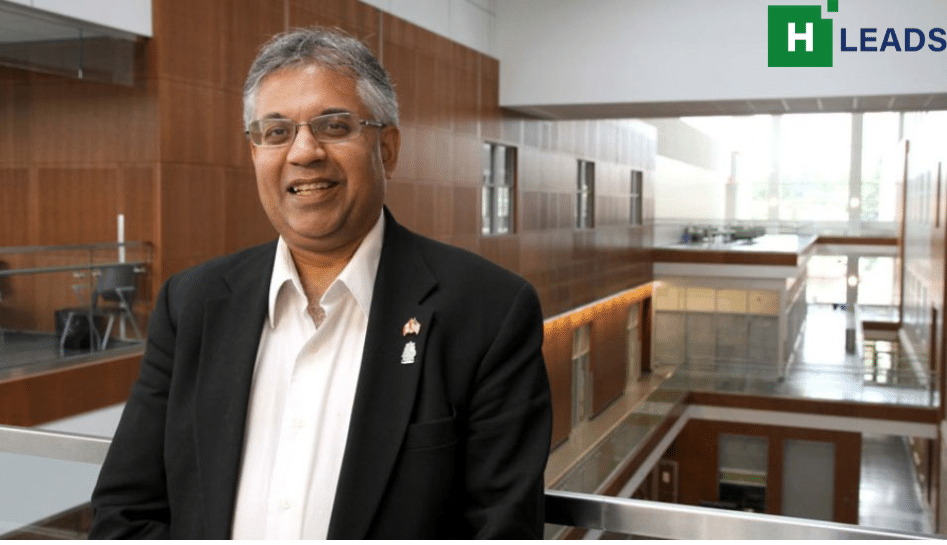
Dr Kishor Wasan is a Co-Director and Co-Founder, Neglected Global Diseases Initiative at the University of British Columbia. He is credited with developing an oral formulation of the old antifungal drug Amphotericin B, which is used in the treatment of blood-borne fungal infection. The drug was subsequently also found effective in the treatment of leishmaniasis, a devastating disease which affects those living in poor sanitation conditions.
In a conversation, Dr Wasan tells Shruthi Manjula Mohan that COVID-19 pandemic has been both a boon and a bane for Neglected Tropical Diseases (NTDs). Boon, because people have realized that the magnitude of NTDs is much greater than the resources dedicated for its prevention. And bane, because everyone has spent the last two-three years in research and development for COVID, leading to further neglect of NTDS.
“Resources dried up, the priorities changed for the whole medical fraternity during COVID pandemic. Most of us have pivoted back, but with the lessons of a pandemic,” he said
Excerpts from the interview:
What was your childhood like and what kind of influence did your parents have in the growing up years?
A great influence, I would say.
Both my parents are from India. My mom is originally from Delhi and my dad was from Kashmir before the India-Pakistan partition. In the late 1950s, they immigrated to Canada. We grew up in Canada but always had a foot in India. My parents were both academics. My dad was actually a PhD in statistics and probability. He was a math professor at the local Queen’s University. My mother is a pathologist, an academic at the university, a researcher, as well as a medical doctor. So my formative years were pretty influenced by them. As a child, I watched them and hung around at the university and even started working at a hospital lab which got me really excited about pursuing research in my own career.
Not only that, I actually come from a family of medical folks; my brothers and my younger sisters are medical doctors.
You’ve held multiple positions; first as a faculty, then as an associate professor, different positions as chairs of different programs, an editor. Of all these positions, what remains close to your heart and why?
My favorite position was being a professor at the university where I had my own research lab and then taught undergraduate students. I was in pharmacy school, teaching students, postdocs and also inspiring undergraduate students who wanted to pursue research and science. Those were my best times and probably when I reflect back on my career, these were the most productive times of my career.
I’m on a joint grant with colleagues at Quebec City where we are working on prostate cancer and pancreatic cancer. Though in a senior role now, I think the greatest part about being a research scientist is that you get to interact with people from around the world and unite for a common goal – science. That was the best time of my life.
What are you currently working on?
Currently, I’m leading a special issue in Frontiers in Pharmacology to try to identify researchers who are doing novel therapeutic targets for neglected tropical diseases (NTDs). Three of my co-editors are from different parts of the world, one is from Peru, one is from Pakistan, one is from Congo and then I’m from Canada. That’s a great example of science cutting through borders.
The COVID-19 pandemic has served as a reminder that science communication needs to be simplified for common people in order for everyone to grasp. What is your comment on that?
The pandemic has reminded us that developing new vaccines or therapeutics for infectious and emerging diseases is the need of the hour. Though the warning signs of a pandemic have been there for the last 20 years, but not many resources were deployed into developing vaccines or therapeutics for emerging infectious diseases. Everyone in the space of science was really holding their breath till a pandemic disrupted the world. In fact in 2015, when Bill Gates made a comment that the next pandemic is around, we in the scientific community had been saying this since the early 2000s.
Strangely, we scientists are very good at talking to ourselves and talking amongst ourselves to communicate science and research but we are still never trained to be communicators at a level that can take really complicated information to make it easy for the general public to understand. So the trick is to find a fine line in simplifying science but without misrepresenting what the science is actually saying.
We’ve known for years how vaccines work and what vaccines can do and what are the pros and cons of vaccines. Everyone in the science community understands this but when translated for the general public, some of the message got lost for a variety of reasons and led to misinformation and misunderstanding. .
So, the science community has to do a better job in communicating without the science being lost or misrepresented.
Do you think as a science community we are prepared for the next pandemic if and when it breaks out?
That’s a very difficult question to answer, because we will never know. The awareness has definitely increased after the COVID-19 pandemic. Scientists are definitely at the top of their game, provided funding for their research keeps flowing. Most of the health systems that rescued us during COVID-19 pandemic were built over at least two decades. For instance, mRNA (messenger RNA) vaccine or the platforms used for delivery of some of the vaccines was being developed for diseases such as cancer. So when COVID hit, the healthcare systems pivoted their science.
So to answer your question, I think scientists do have the fundamental building blocks and strategies if a new pandemic hits us.
The COVID pandemic has reminded us that we have to modernize our tools of communication. How important is it to revamp our communication tools?
Well, yeah, I think you’re absolutely correct. I think what we need to do is increase the public service announcements, public service presentations, webinars and more face-to-face conversations with the public. Communication is a superpower, we’ve got. To communicate through all the mediums that we have, is a key. Scientists tend to talk great with each other and that’s how you get collaborations and you communicate your work, but we need to do a better job in communicating by talking to non-scientific folks in the general public because that’s ultimately who we serve. So that’s what we should be doing on a regular basis. The world is much more educated today than they ever have been in their whole history of the world. People are very smart and people have easy access to presentations and the web.
We often see that NTDs don’t get the spotlight that they deserve and they are left behind in the larger conversation except for HIV, AIDS, tuberculosis and malaria. Why do you think that happens and how can we build better systems to enable conversations around them?
I think there are two main reasons why NTDs are neglected.
I think number one is that these diseases are showing up in low and middle income countries and places around the world that the west doesn’t focus on. It’s not that they house any malicious intent or anything at all. It’s just that it’s not on their radar?
Number two, there’s a lack of resources put in for the magnitude of the disease such as NTDs. COVID affected everybody differently and didn’t have any barriers. It was an indiscriminate disease and it hurt everybody in different ways. It led to alarms but what has happened unfortunately because of this governments have become more insecure and decided to take care of themselves first. In fact, unfortunately, the funding for NTDs as well as other humanitarian work done by Doctors Without Borders and other humanitarian organisations has been cut in the most recent budgets in Canada and the UK. More resources have been devoted to what is happening locally or within the nation.

Has the COVID-19 pandemic been a boon or a bane to NTDs?
The pandemic has done two things for NTDs, one positive and one negative. On a positive front, people have realized that the magnitude of NTDs is much greater than the resources dedicated for its prevention. The pandemic has increased awareness about the emerging infectious diseases that were probably neglected all this while. During the pandemic, we were able to mobilize the community, we rallied around coming up with vaccines and therapeutics for COVID so quickly, which by the way was built over 20 years of research. Today, the medical world is more prepared with tools and strategies for preventive diseases.
The negative is that because everyone has spent the last two-three years in research and development for COVID, this has led to neglected diseases, being neglected more and taking the backseat. Resources dried up, the priorities changed for the whole medical fraternity. Most of us have pivoted back, but with the lessons of a pandemic.
What do you think is the economic loss for a country if NTDs are not addressed
Oh, it’s huge, because millions and millions of people are infected, millions of people’s people’s livelihood is taken away. Let me give you an example; So one of the NTDs that I work on is leishmaniasis. It is a devastating disease which affects those living in poor sanitation conditions which attracts sandflies who’s sting releases a parasite and ultimately if you’re not treated you can die from leishmaniasis.
This disease is found primarily in rural communities. And usually, the people that are most affected are the rural workers and it’s usually women of childbearing age and children themselves who bear the brunt. If someone who’s working in the field or their children get infected, it completely affects their ability to work and leads to a huge economic burden on the local community, which trickles up to a national level.
With NTDs you are not dealing with a few people but a few hundreds of millions. We have under-reported these diseases.
Health misinformation often stands in the way of healthcare, especially when it is faith healing, miracle treatments. How does this affect NTDs?
I think the answers are yes or no. I think as long as we are developing and doing research in science, I don’t think there’s an issue with misinformation because it’s still isolated. But once we get to a product or we get to a technology or new standard of care and want to get it on to the ground at the local level, that’s when the problem starts. People are hesitant, they’re scared of the unknown and that’s when misinformation starts to trickle in. Back in the day, you know news was news. It didn’t matter which channel you were watching, or which paper you were reading. If it was a fact, everybody spoke of the same fact. Today, facts and opinions have all got mixed up. The general public has to be very careful about what they read, what they see on television, what they see on streaming sites, what they see on social media platforms, and have to unfortunately, figure out for themselves.
How can the governments support more research and development for NTDs?
We have this wonderful organization in Canada called the Canadian Network for NTDs, it’s a group of academicians and NGOs located in the capital of Canada, Ottawa. For the western world, NTDs remain ignored since it doesn’t affect them and that derails the funding and resources. Well, the reality is that our worlds are so interconnected now because of air travel and other means anything that effects one part of the world can certainly have an effect on other part of the world, COVID is an example. The last time the world was hit with a pandemic was in 1918 with the Spanish Flu, which was a devastating disease but it didn’t travel as much as COVID did. It was much more isolated.
So the way is to convince governments that if NTDs are not addressed then it could end up at your doorstep sometime and it could affect us in a number of ways. For example, if a country has trade agreements with another country affected by NTDs, then the business will be affected. There indeed is an economic loss to this situation.
I realize that you are a big fan of a collaborative approach. Can you cite examples from your experience and the techniques of collaboration that made the most sense to you?
Oh, there are so many of them. Let me give you an example of leishmaniasis. I developed an oral formulation of the old antifungal drug Amphotericin B, which is used in the treatment of blood-borne fungal infection. So these are infections that occur in patients that have a poor immune system. These patients are at the risk of contracting HIV or uncontrolled diabetes or cancer or could need organ transplantation. They have a weak immune system and could contract a fungal infection that could kill them.
In that case, Amphotericin B is a wonderful drug to treat that infection. However, it’s got limitations and the big limitation is that you have to administer it as an injection. It’s also cost intensive and only a trained healthcare worker can administer the infusion. Some physicians were using it as a preventative therapy where this was administered to patients before their transplant, for instance.
So I had doctors who suggested that I develop an oral formulation of Amphotericin B, in a non-injectable form, that’s cost-effective and that is tropically stable so you don’t have to put it in a refrigerator. And that is also accessible and affordable for rural communities. So we developed something for this fungal infection, published our papers and then out of the blue, I received a call about using this to treat leishmaniasis, a parasitic disease. They needed something that was cost-effective, that was safe, that was tropically stable, and accessible in rural communities.
Eventually we gave a presentation to the Bill & Melinda Gates Foundation, which is down the street from us in Seattle and they partnered us with a group in Ohio, who had an animal model for leishmaniasis. So we went and tested our oral formulation and it was very effective. In fact, it worked better than my antifungal models. And that led to the new collaboration in developing an oral treatment for leishmaniasis. We finished phase one of clinical studies, safety studies to show that our formulation is safe and now I’m working very hard to get it into what we call efficacy studies, which is the phase-2. So this is what I call a collaboration that elevated the primary idea. So today, I’m working with MSF Canada, DNDi, WHO, and a group of clinicians in East Africa.
Also Read: ‘Private healthcare dominates India’s medical landscape’
















Add Comment