Connected diagnostics not only streamlines healthcare workers’ access to accurate data in private and public settings but also leverages technological advancements to integrate documentation of diagnostic and treatment goals
Imagine this – you go to your local doctor in a primary healthcare facility in a tier-2 city to get help with this niggling cough that you have had for days. Is it COVID-19? Is it the flu? You are asked to visit a public diagnostic center or nearby hospital to get tested for COVID-19, perhaps a private one in another town to get a chest x-ray. You now go back to your doctor with their prescription, along with two different envelopes with your results, or maybe you get the reports on your phone through different apps.
But what if we could integrate this information and make the diagnostic and treatment process more streamlined and responsive to the needs of diverse healthcare systems and people? How could this make the response to the next outbreak (or surveillance on a current one) more effective and equitable?
In the last couple of decades, we have seen an immense growth in healthcare related innovations – diagnostics, devices, therapeutics, vaccines, digital health. However, if the COVID-19 pandemic has taught us anything,… Share on X
While initiatives such as the Access to COVID-19 Tools (ACT)-Accelerator shed light on the incredible impact global collaborations can have on information and technology sharing, the reality is that access and uptake are not equal. Hence, diagnostics must be expanded beyond pandemic preparedness, a key element of our goal of achieving and ensuring access to universal healthcare.
Connected diagnostics can play a critical role in ensuring that the challenges associated with global biomedical research, response, and prevention are addressed.
What are connected diagnostics?
Accurate diagnostics for the detection of pathogens, something capable of causing disease like a virus or bacteria, is crucial in informing public health responses and controlling any disease before distributing any therapeutics for treatment or vaccines for prevention. Yet, diagnostics does not exist in a vacuum – it requires well-linked laboratory, disease surveillance, and health information systems capable of using this data in effective ways. This is where connected diagnostics comes in.
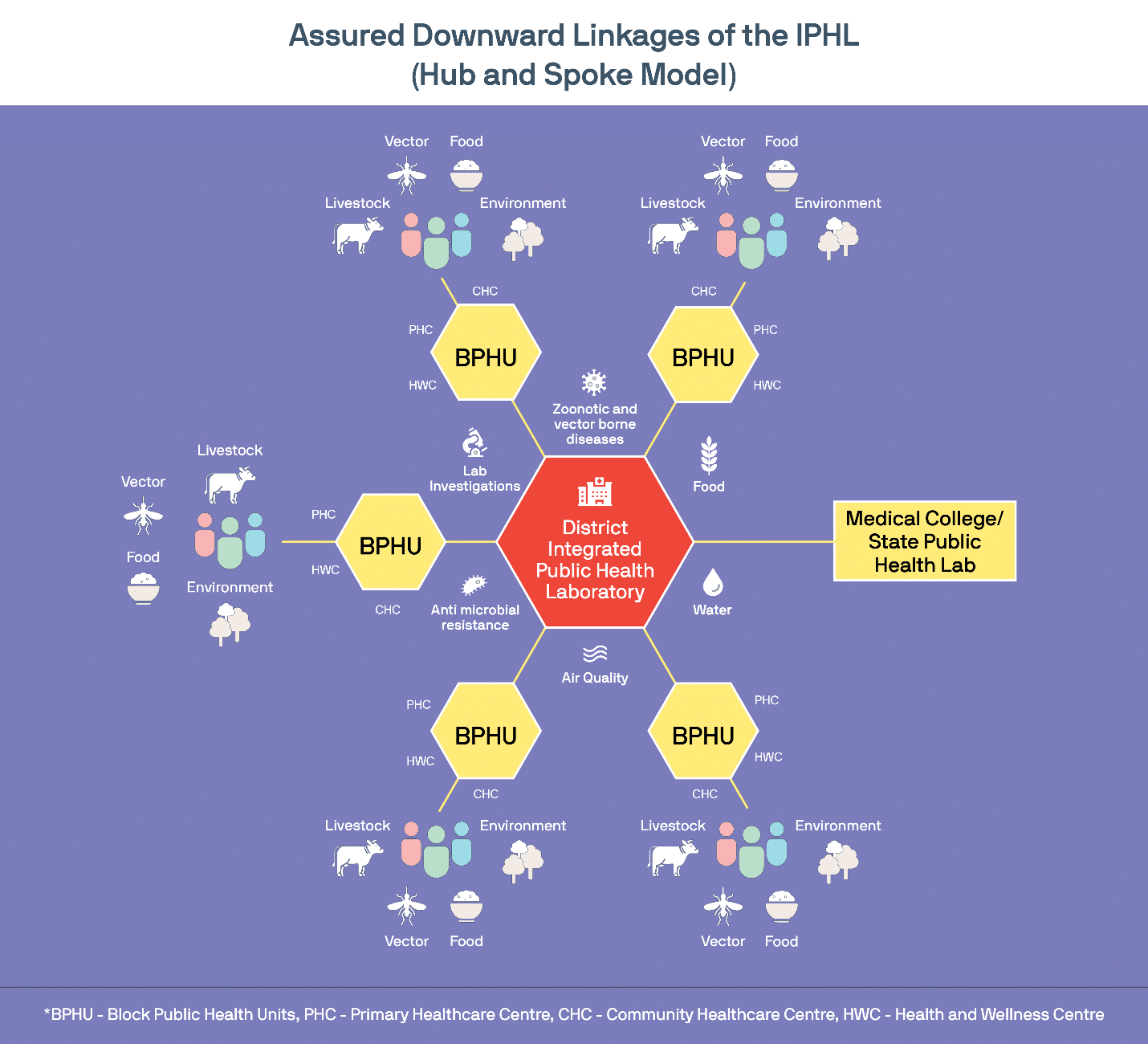
Connected diagnostics are basically those system which are digitized for the purpose of adapting and integrating with the broader healthcare ecosystem. They can include health record systems, m-health applications, and lab surveillance networks, among others. Take the Ayushman Bharat Health Infrastructure Mission as an example. The programs’ goal is to scale up an IT-enabled disease surveillance system by developing a network of public and private surveillance laboratories at block, district, regional and national levels to effectively detect, monitor, and prevent public health emergencies. Launched in the wake of India’s massive COVID-19 response, this effort seeks to fill existing gaps in the healthcare system which the pandemic exacerbated and integrate primary, secondary, and tertiary levels, thereby strengthening efficiency, timeliness, accessibility, and equity of health services across the continuum of care.
Opportunities abound
Connected diagnostics not only streamlines healthcare workers’ access to accurate data in private and public settings but also leverages technological advancements to integrate documentation of diagnostic and treatment goals. For instance, mobile-based health applications which can be used by clinicians, healthcare workers, patients and their families. It also helps in optimizing clinical care processes and procurement of resources. Most importantly, by ensuring that health-related data is made available to communities regardless of where they are, connected diagnostic systems have the potential to empower patients to facilitate their own health-related decision making, one which reflects their values and preferences in a holistic and bi-directional manner.
“However, there are some critical challenges which must be overcome in the process. This includes addressing data security and confidentiality; low data and digital literacy among patients and healthcare workers; lack of basic infrastructure to facilitate this pivot to the digital; and lack of enabling policies at a global scale which address issues of data ownership, among others. “
Also read: Penetration of telemedicine in India is far below its potential
The development of global policies to fully incorporate multi-sectoral needs across the continuum of care are still underway. One example of this is Transform Health – a global coalition of organizations committed to harnessing the power of digital technologies and accurate data to transform and strengthen primary healthcare. The coalition developed a global health data governance framework – comprised of three basic principles to protect people, promote health value, and prioritize equity – to ensure the maximum utility of national and regional health data while protecting individual rights.
Similar collaborations are critical to the successful workings of collaborative diagnostics. This collaboration must take advantage of the networks and partnerships that have been put into place at all levels during past epidemics and pandemics – such as HIV and TB – and learn from what went wrong and what went right. Finally, with an increased use of digital tools to support community education and public health responses during the pandemic, we must be mindful and adopt approaches such as trust building, community engagement, and effective and empathetic communications to truly encompass our goal to leave no one behind.
Also read: Not just prevention needed to fight dengue in India


















Add Comment